Signs & Symptoms Signs Doctors Look For Making the diagnosis Surgery Management Support
Why is it that, one of the questions we have found most useful in the diagnosis of endometriosis is … – “did you miss school as a young girl because of your periods?” Often, these patients are now in their 30’S and 40’s! So often the answer is “yes” – and they now miss time off work as well.
These women have often been
silently struggling for years
- they have been to the
doctor at 14 or 15 years of
age and have been told things like:
It’s just women’s business
Periods are meant to be like this
Your mum had it, so that’s probably why your periods are painful
You’ll grow out of it
It’ll get better when you have babies
Go on the pill
Or later, let’s change your pill
Inability to move bowels at period time because of pain with bowel movements
Pain with intercourse – “nature” is trying to reproduce the species – why would nature make it painful!
Family history of known endometriosis or terrible periods (Mother, Sister, Aunt)
Blood in the bowel movements, coughing up blood, nose bleeds – only at the time of period (these are some and of course could have other causes)
Loose bowel movements at period time
Pain when moving bowels at period time
Having had half a dozen (normal) ultrasounds, despite ongoing pelvic pain
Presenting to the doctor and saying: “I have been on numerous Pills and still spot all the time, even when on the pill”. Doctor says “let’s try another one”. Wrong answer
Pain with periods
Heavy periods
Clotting with periods
Having to have time off school or work
Bleeding between periods
Bleeding with intercourse
Pain or frequency of urination (worse at period time and often misdiagnosed as a urinary tract infection
Abdominal bloating
Making the Diagnosis
Doing a laparoscopy, or in the past a laparotomy, is the only way the diagnosis can at present be confirmed. A laparoscopy involves:
1) A day trip to hospital and a general anaesthetic
2) 3 or 4 small incisions in the abdomen
3) 3-4 days off work
Signs doctors look for
Abdominal bloating
Specific tenderness in the “Pouch of Douglas”
Specific “point” tenderness on one side high up in the vagina at the time of vaginal examination
Inability to confidently feel an ovary as a separate entity (because the ovary is attached to the lateral pelvic side wall)
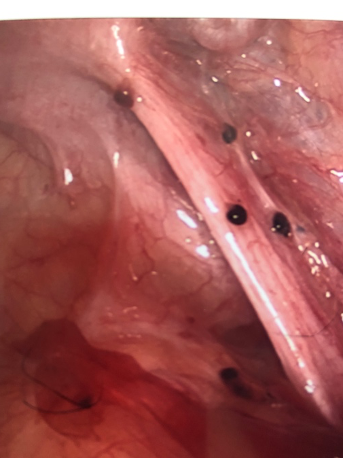
Endometriosis on laparoscopy
Endometriosis on laparoscopy
Management
If endometriomas are small, they should be excised (not just drained) completely at the first operation. If they are larger than 3cm in diameter, my approach is to drain them and then treat the endometriomas medically, before going back in to carefully excise the capsule. The goal here is to decrease the risk of serious adhesion formation.
Medical Treatment
Any disease in medicine where there is a plethora of treatment options and variability in disease, points to the fact that there is no perfect treatment – (arthritis is another example of this). Sometimes, the available options need to be trialed so that the correct medicine and even the correct dose of that medicine is obtained to suit the patient’s needs. Sometimes more than one medicine may be needed concurrently eg. the pill and added progesterone.
THE AIM OF MEDICAL TREATMENT IS TO STOP THE PERIODS!
By doing this, bleeding is also stopped into the “blood blisters” of disease in the pelvis and other areas, which is actually the endometriosis.
The Use of Ultrasound in the diagnosis of Endometriosis
Really, the only time an ultrasound is useful is if large lumps of endometriosis are seen, if the vaginal probe hurts (it shouldn’t), or if an endometrioma (ovaries filled with old blood caused by bleeding into an ovarian cyst) are present. In expert hands the bowel stuck to the posterior surface of the uterus can be detected but this requires a skilful experienced technician
Surgery to diagnose endometriosis
I always take a lot of photos of the surgery as I think this is a useful way of showing my patients the extent of their disease. They are also useful for me, for future reference. It allows me to see whether the disease has, in fact, regressed with my treatment. Digital images can also be sent to other Endometriosis Specialists, either interstate or overseas should the patient relocate.
The great thing about modern day laparoscopy is that the laparoscope actually becomes a mini-microscope – because of the excellent optics and picture quality available the end of the laparoscope, it can be pushed right up almost adjacent to the part of the pelvis that is being examined.
Step 1
Anatomy is identified after instruments are inserted into the pelvis.
Step 2
To do this a laparoscope is inserted through a trocar (pipe).
Step 3
In particular, the course of the ureter is traced, because if the ureter is damaged, a 2-3cm hour microscopic re-anastomosis needs to take place – this happens through an old fashioned cut in the tummy in many instances and would mean several days in hospital and a month to 6 weeks off work – obviously we do not want to hit the ureter.
Step 4
The best way not to damage a ureter is to dissect it out. I start well above the diseased area, especially when the disease is over the ureter directly. It is best to start dissecting in normal tissue, because it is not scarred, and tissue planes are easy to identify.
Step 5
The area of endometriosis to be excised is picked up with laparoscopic grasping forceps.
Step 6
The area is excised by using a cutting and if needed coagulation current, applied through a “spade” or spoon tipped instrument. The harmonic scalpel can also be used here. If any small bleeding vessels occur, a bipolar tipped instrument is used.
Step 7
An endometrioma, that is a blood filled ovarian cyst with a thick capsule or wall, must be adequately treated or it will simply come back within months.
Tubal Endometriosis
The surface of the tube is not uncommonly affected by endometriosis It is difficult to excise tubal endometriosis without permanently damaging the tube. For this reason, this is one area where I just gently burn it off (ablation).
Endometriosis may also exist in the lumen of the tube, out of reach of the surgeon. A fallopian tube partially blocked by endometriosis, may lead to a tubal ectopic pregnancy (see Surgical Gallery).
Emotional Support
Please see the links in the ECCA endometriosis care centre Australia or QENDO (qendo.org.au).