Infertility, should in most cases be referred to as ‘sub-fertility’ because of the changes made in ART (assisted reproductive technologies). That said, we classify infertility/sub-fertility as ‘a couple who have failed to reproduce after 12 months of regular intercourse’.
The “average” couple will
conceive by the 4 months’ mark.
Male Fertility
Female Fertility
Age Factor
The Initial Infertility Consultation
Physical Investigations
Later Investigations
General Recommendation
Male Fertility Preservation Recommendations
The “average” couple will conceive by the 4 months’ mark. However, with women (and men) now electing to delay pregnancy, sometimes into their late thirties and early forties, I personally start the investigative process much earlier than one year, provided they have a referral from a GP to see me.
Male Infertility
Causes of Infertility – Male Factor
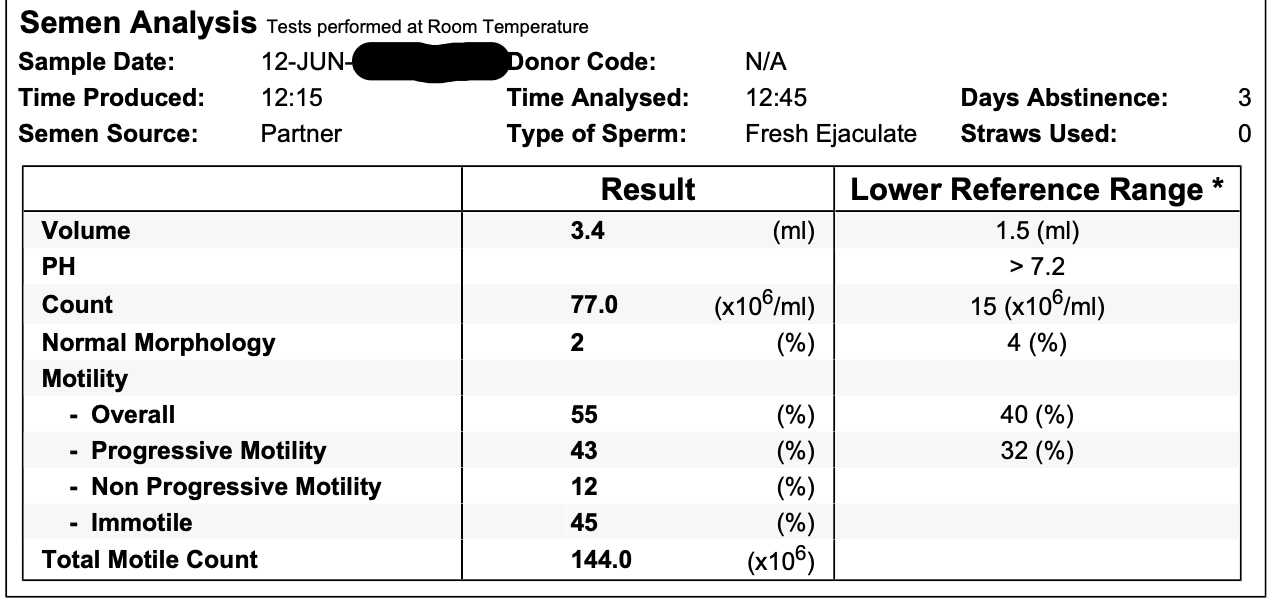
The first investigation I always suggest is a semen analysis. Abnormal sperm counts account for approximately 50% of causes of failure to achieve a pregnancy in 12 months. Gone are the days where sperm counts were done as the last resort. I encourage couples to have this test early.
Even in some cases, when a semen analysis has been ordered before by another laboratory and were said to be normal, I always insist on sighting the previous report, repeating the analysis, and using our expert scientists at City Fertility Centre (Brisbane)
Below are two examples of a Semen Analysis done through City Fertility Centre:
A normal count, showing normal surrounding cells. There is normal morphology (the sperm look structurally normal) and there is normal motility. There is also good survival over 24 hours.
An abnormal analysis that shows poor numbers, poor morphology, decreased motility, and decreased survival is shown.
NORMAL SPERM COUNT
ABNORMAL SPERM COUNT
Why do I insist on a second sperm count?
Too many times I have been told that the sperm count was reported as normal, however when reviewing the report to see that the number of sperm was normal but they were not moving properly and/or not normal in appearance
The vital diagnosis of anti-sperm antibodies (causing severe clumping of the sperm with failure to fertilize) was missed because that part of the test was not ordered. I always make sure that I order an anti-sperm antibody on the CFC request form.
Treatment for abnormal sperm counts can be at several levels
Firstly, if the count is proven to be abnormal, we always suggest a repeat test 4-6 weeks later. Such things as severe flu in the 2-3 months prior to the test (the life cycle of a sperm is approximately 70 days), can cause an otherwise apparently normal male to have an abnormal sperm test.
Lifestyle and dietary changes – I suggest that patients
- do not smoke, or drink alcohol
- reduce caffeine intake
- drink plenty of water, sleep well and exercise
- do not take steroids
- include a vitamin C and zinc supplement with a healthy diet
If the sperm count, morphology or motility is only down slightly, or there is mild to moderate clumping, we suggest Artificial Insemination, where the semen is washed with concentrated 60% ‘pure sperm’ (a proprietary product or something similar), therefore selecting out morphologically normal sperm and also making them swim better and live longer!
The prepared semen sample is inserted into the uterus using a small cannula (small soft flexible pipe) - the sperm is drawn up into a syringe and on a predetermined day (ie. day of ovulation), the sperm is directed into the uterus.
This procedure is performed in the City Fertility rooms and is not painful but may be mildly uncomfortable. I have achieved a pregnancy rate of about 15% per attempt over the last few years (as per City Fertility Centre data). This is compared to a natural success rate of about 25% when two people initially try to reproduce. Therefore, I usually suggest 3 or 4 attempts at artificial Insemination, before going on to IVF, provided that the tubes have been proven to be open, and the semen analysis shows only mild to moderate abnormalities.
Severe Semen Analysis Abnormalities
Often, problems with the female (such as blocked tubes, endometriosis, polycystic ovaries etc), co-exist with sperm problems in the male partner.
Here, there is no question that the couple should be offered IVF treatment. A decision needs to made if the treatment be standard IVF or if ICSI is needed (Intracytoplasmic Sperm Injection). ICSI, where a single sperm is injected into a single egg, is certainly the treatment of choice for previous failed fertilization during an IVF attempt.
Severe sperm antibodies, can exist even in the presence of a normal number of sperm and normal morphology and often occur with previous vasectomy reversal, and trauma to the testicles.
Female Fertility
Cause of Infertility – Female Factor
Tubal Disease – The fallopian tubes are like a flexible pipe, allowing sperm to reach the egg. Damage to one or both fallopian tubes can occur with ascending infection (most commonly STD’s such as Chlamydia), peritonitis caused by appendicitis, tubal ectopic pregnancy causing rupture, removal, or surgery to the tube.
Once the fallopian tube is damaged internally, there is not much that can be done, despite previous hope that lasers for example, might be able to re-bore the tube. This has not eventuated. If the damage to the tube is external, eg. by adhesions, and the internal anatomy has been spared, there is some chance that once the “kinks” in the tube, (caused by the adhesions pulling on the usually flexible fallopian tube, and distorting it), that fertility could be restored. To fix this needs a laparoscopy of course, with careful dissection of tubal adhesions.
Ovulatory Problems
The most common cause of women failing to ovulate is seen with “polycystic ovaries” – there is much confusion in literature about this topic, and the cause of the problem is still not fully understood. There is however, a hereditary component.
Professor Gab Kovacs has written an excellent book on polycystic ovaries which was published in 2000 (ref; Polycystic Ovary Syndrome edited by Dr Gabor T Kovacs, Monash Medical School, Box Hill Hospital, Melbourne, Australia, Published by Cambridge University Press 2000).
Suffice it to say this is a spectrum of disease with at one end “polycystic ovary syndrome” per se with symptoms characterised by an excess of androgens, or male type hormones (including testosterone). These hormonal imbalances cause dysfunction to a woman’s menstrual cycle, and because of inappropriate levels of hormones, the egg follicle (egg cysts) in the ovary, have difficulty even developing. They arrange themselves like a ring of pearls around the periphery of the ovary. Therefore, periods are long and ,unpredictable and irregular and ovulation is infrequent .This makes timing intercourse for reproduction very difficult.
Common symptoms of the full polycystic ovary syndrome (as opposed to a mere ultrasound diagnosis of polycystic ovaries, which may occur in up to 20% of normal young women), include the following:
Excess hair growth (most noticeable on the face and chin)
Acne
Obesity
Menstrual disturbances (very irregular and long periods)
Infertility
In extreme cases male pattern balding
Abnormal glucose tolerance test
Abnormal lipid profile
The Age Factor
When is it too late to have a baby? When is it too late to try? And, when is it too late to consider IVF?
There are no hard and fast rules here. Suffice to say however, that the older the ovaries are (not necessarily the older you are), the more likely you are to:
Have trouble ovulating
Have trouble producing a good quality egg
Have trouble keeping the embryo, even though it does implant
Miscarry – miscarriage rates in the 40+ age group are reported to be 50%
Need an amniocentesis to exclude the possibility of a chromosomal disorder (such as Down’s syndrome)
The amniocentesis(where fluid from around the foetus is taken and sent for chromosome analysis), has now been replaced by the nuchal fold thickness test, and or the Harmony blood test.
However, having mentioned age, I recently delivered a 46 year old woman who conceived with IVF technology. She got the donor eggs from her 24 year old daughter and she was pregnant after the first cycle. This is obviously a personal choice. Here it was the age of the daughters eggs ,not the age of the mother, that allowed her to conceive easily.
Donor Eggs are also available from City Fertility Centre and several overseas counties including South Africa, Greece, and Turkey . Please discuss this with me if this is your choice.
There are numerous other causes of infertility, too numerous to discuss in detail here. These include congenital, anatomical variations, endocrine diseases and premature ovarian failure ,deep infiltrating endometriosis, adenomyosis (covered elsewhere).
The Initial Infertility Consultation
If possible, try to be present as a couple. I find that if the partner is present, I am more likely to have success in obtaining a semen sample, from previously shy husbands or partners (husbands will not of course be asked to produce a semen sample on the day, but rather will be sent away with a request slip. Similarly ,same sex couples should come together.
A full medical history will then be taken from the male and female partners. Important details include the regularity of the females menstrual cycles, pain with cycles, how long you have been trying, and have you been trying on the right days. Have there been any previous pregnancies, medical illnesses, has there been past surgery? Are you on any medications, alcohol, tea, coffee or drugs? Has a pap smear been taken? I also ask for a past history of any chlamydia or gonococcal infection.
In the male, we are particularly interested in injuries to the testicles, work place ,or home chemical exposure, and drug exposure, especially to steroids, caffeine exposure, alcohol and smoking history, history of infections as child such as mumps or operations on undescended testes as a child The family history is also important here. In the work place males, more than females, can be exposed to glues, resins, paints, dusts and other toxic fumes. I will also suggest that both males and females avoid cleaning products that lurk under the kitchen sink!
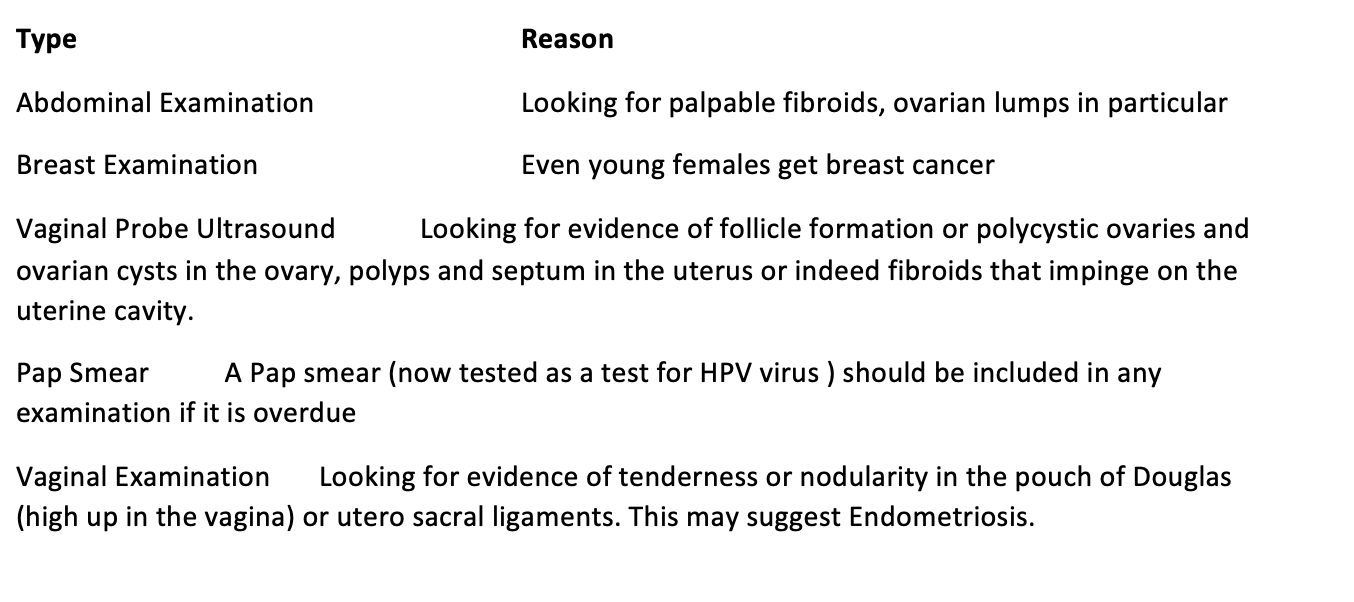
Initial Physical Investigations in the Female
Initial Physical Examinations in the Male
If there are any physical abnormalities admitted to by the male on questioning (because I am not urologist) I will usually refer the male partner off to one of our specialist urology colleagues. This is particularly important in erectile problems, ejaculation problems, past history of undescended testes and if there is likely to be a need for aspiration of the sperm under general anaesthetic and for IVF purposes. Having said that, I quite commonly aspirate the sperm from the testicle under general anaesthetic myself, when indicated ,for an extremely low sperm count
Initial Laboratory Investigations
Later Investigations
Laparoscopy
Unless there are obvious symptoms of endometriosis, I usually wait 3-4 months before offering laparoscopy. This involves a day trip to a hospital, usually a brief anaesthetic, at least 3 punctures in the abdomen, sometimes 4. Insertion of a 10mm telescope or a 5mm telescope through the umbilicus, to view the content of the pelvis.
Hysteroscopy
A hysteroscopy is done at the same time as a laparoscopy, is cost effective regards to time, trips to hospital, anaesthetic costs, pain (very little pain). An endometrial scratch is also to be done at the time of a hysteroscopy in those patients wishing to try to conceive. There is debate about whether an endometrial scratch actually works.
Dye Test
Dye is put in through the cervix and i watch with the laparoscope to see if it flows out through the fallopian tubes. If dye comes out through the fallopian tubes, the tubes are said to be open (Surgical Gallery).
Note: If any problems are found in the pelvis at the time of laparoscopy, and in my professional opinion as a surgeon these can be easily and safely operated on at the time, then they will be dealt with at the time of surgery. It is pointless waking you ,the patient, up to discuss this when it could easily be done in one operation.
Hysterosalpingogram
Hysterosalpingogram was a common test for tubal patency in the days before laparoscopy. The test is not pleasant, being performed in the X-ray or ultrasound department, without anaesthetic.
I reserve it for cases where the tubes looked normal at laparoscopy, but I could not get any dye through the tubes. Occasionally this can be due to tubal spasm and the tubes do look otherwise normal. It is important to inject the dye slowly at laparoscopy and this usually avoids tubal spasm.
Sonohysterogram
An even better test is the use (by a competent and experienced scanning person )of the ultrasound scan and an ultrasound “opaque dye”, which is inserted up through a small urinary type catheter, into the cavity of the womb. The ultra-sonographer then waits for the “spill” of the fluid to be seen on ultrasound.
Artificial Insemination
This is also called Artificial Insemination(“AI”) or Intra Uterine Insemination (“IUI”). This involves carefully and gently inserting prepared sperm produced by the male partner, or thawed donor sperm, up into the uterine cavity, at the time there is an egg present on the ovary.
Usually this is done because of a sperm problem – low numbers, low mobility or a decreased number of normal looking sperm. It is also performed when the “raw” sperm has too much clumping – clumps of sperm which cannot then move in a straight direction towards the egg.
So, what will happen? How will I prepare you for Intrauterine Insemination?
In order to be sure that we do not waste another month, we suggest a small dose of Clomid or Letrazole (starting at just ½ a tablet a day and going to days 2-6 of a cycle). You will be asked to ring on day 1 of your cycle (day 1 of bleeding) and make an appointment to see me on day 12 or your cycle if you have a 28 day cycle. If, for example, you have a much shorter cycle, I will see you earlier. If, however, you have a 35 day cycle, I will ask you to come in on day 18 or 19. We want to get to the ovary before it ovulates.
On that day 12, I will perform a vaginal ultrasound scan, and if there is an egg follicle present and it measures >1.3cm, an injection of HCG will be given. This injection has no known side effects and mimics the body’s LH surge (HCG and LH are so similar that the body cannot tell the difference). In this way, we can induce ovulation at a definite time. HCG (as the trigger) to ovulation also primes the endometrium so that if you do become pregnant the lining is more receptive to the tiny embryo. I tell my patients it is a bit like putting fertilizer on a garden bed of the uterine cavity.
The following day, (day 13) your partner will be asked to produce a semen sample which will be prepared (it takes about two hours at City Fertility Centre) and one or both of you should bring this prepared sample back to my office. Obviously, I will need the female partner! In a procedure very similar to a Pap smear, the prepared semen is delivered into the “cavity” of the uterus, through a very thin flexible pipe. This takes less than 5 minutes and is associated with no more discomfort than a Pap smear! There is then a wait of 2 weeks to see if you have conceived.
Generally, I recommend no more than 4 IUI cycles. In my hands, most couples conceive after 4 cycles and if conception has not occurred by then (remember, you have usually already been trying for a year or more) I would suggest an IVF cycle. This often becomes a test of fertilisation ie what does happen when your eggs and sperm meet. For example, the scientist will look for sperm binding; is there good or poor sperm binding – how many eggs did we get and how many actually fertilized. What is the quality of the embryos, do they reach day 5 blastocyst stage and are any of them able to be frozen. All these are important things to consider.
General Recommendation
An acknowledgement that health professionals working with patients who are at risk of infertility from cancer therapy are recognisant of the importance of future fertility for this patient group and that the preservation of fertility is as an important part of the cancer journey for these people. It should be further acknowledged that while all effort should be made to preserve the fertility of this at risk group a number of ethical and legal parameters should be outlined to further shape the development of this emerging area of oncofertility. A consensus of these parameters should include:
All patients who are to receive conventional cancer therapy be given the opportunity in a timely manner to discuss their fertility in the setting of cancer therapy whether they are deemed at risk or not. (This should include the opportunity to speak to an infertility health professional, should they wish it).
The patient should be given realistic recommendations about the likely success of preservation methods, including the risk associated with undergoing the procedure in the setting of their cancer diagnosis.
Where possible the patient is given appropriate time and information to contemplate their decision to come to satisfy the rigours of informed consent.
Evidence should be used to determine the risk for infertility for the patient and that a reasonable view of the long term survivorship for the patient should be weighed against the decision to withhold treatment, reduce initial intensity or defer sterilizing treatment.
Clinical evidence, coupled with a risk profile should be used to determine the best preservation method to be used to improve the protection of or storage of gametes.(gametes are eggs and sperm ).
Given the generational nature of study into fertility preservation, it should be recommended that a decision to use experimental preservation methods should neither be precluded from use in patients who have a high risk for infertility (>50%) nor should they be actively encouraged outside the remit of clinical trials where possible.
Hospital ethics committees should be engaged to assist decision making for either generic recommendation for experimental fertility preservation or on case by case basis, particularly in the setting of those under the age of consent.
Support for current clinical trials or the development of new clinical trials should be supported by both hospitals treating cancer patients and assisted reproduction clinics.
Male Fertility Preservation Recommendations (Prior to chemotherapy)
Initially
All pubertal males should be given the opportunity to semen cryopreserve by masturbation before cancer treatment, whether or not they are considered at risk for infertility for chemotherapy or surgical treatment.
The patient should be sent a letter as soon as possible from the fertility clinic to outline the quality of the sample and the likely success for use of the sample. This should be done to both, give the male realistic expectations post treatment and to aid further decision making about future fertility.
The use of either testicular aspiration or microdissection for unsuccessful masturbatory contributions or other premorbid conditions should be considered in patients with a testicle size 8ml or larger.
Follow Up
Unsuccessful patients should be sent for a follow up semen analysis, either after the first cycle if well or between other cycles, if appropriate and if semen quality is appropriate, a sample should be banked with a reputable IVF clinic.
All males should have a semen analysis done 6 months to 2 years after cytotoxic therapy has completed.
Follow up counselling with an infertility health professional should be offered for all patients to discuss their fertility outcomes, not matter what the outcome.