Here we enter a potential minefield. On the one hand, you, as a significant other, do not want to see your loved one in pain, but where do you start, and how much analgesia is too much?
Certainly, we do not want to see what I hear repeatedly happen in the hospital system, especially the public hospital sysem. You do not really want to see your spouse or girlfriend taken up to an accident and emergency department in extreme pain, having to wait for hours to be seen by a doctor who might be junior or not aware of these gynaecological conditions. The doctor, thinking they are doing the right thing, does an abdominal or vaginal examination and finds that it is painful for the women when they rock the cervix or tender in the pouch of Douglas.
If the patient is lucky enough, she will get a swab to exclude infection and a scan to exclude a possible ovarian cyst. And if she is really lucky, the doctor, noticing from the history that the pain is cyclical, will refer her to a gynaecologist for a semi-urgent review. The doctor, quite rightly (if done only once), orders an ultrasound, and that takes another one to two hours to get the results. It is likely nothing has been given for pain relief yet!
The results often indicate that the pelvis “looks normal”. That means there is nothing wrong, correct? No, absolutely not.
Endometriosis and adenomyosis are rarely seen on an ultrasound, unless they are in the advanced stages. Certainly, early endometriosis is not seen. So, not really knowing what else to do, the doctor—having checked the white cell count (WCC) and seeing it is normal, therefore ruling out infection, and that the HCG (pregnancy test) is negative—gives the patient a “shot” of morphine intramuscularly (or similar narcotic orally), and then sends her on her way with twenty Endone tablets (the maximum legally allowed to be prescribed at any one time). Endone is a narcotic like morphine, heroine, and codeine.
The pain is pretty severe. On the box it says to take Endone for pain (only when necessary) every three to four hours. Well, it is pretty necessary most days for three or four days every month.
The Endone’s gone. Things are okay for a while or at least until the next period comes. Then the pattern repeats. The next doctor in the accident and emergency department, usually a different doctor this time because they rotate shifts, goes through exactly the same process but is perhaps not as thorough because all of the tests have recently been done, and then sends her home. Still no diagnosis. Still no referral to the gynaecology outpatient department or private specialist. Perhaps they write a letter to the general practitioner, while dispensing stronger (addictive) pain relief.
The general practitioner who receives correspondence from the hospital sees that the ultrasound was normal and quite commonly does not follow up with a gynaecology referral either (either publicly or privately), but instead organises a gastroenterologist appointment, because, by that stage, the belly is so distended and painful because of the narcotics slowing the bowel down and causing “bloating”, that there are now two causes for the pain—possible endometriosis and probable distention from the painkillers. Irritable bowel, as previously discussed, becomes the common misdiagnosis until proven otherwise. The heavy periods with clotting, flooding, and pain have been forgotten.
Six months pass and the patient eventually gets a referral to a gastroenterologist. She gets the specialist appointment, and soon after a colonoscopy, the bowel is normal. The gastroenterologist has not taken a gynae history. They call it irritable bowel.
The patient goes to a different accident and emergency department or general practitioner, again in severe pain. The process is repeated, and more Endone is prescribed and the “irritable bowel” is treated in a different way. But still, because the cyclical bleeding has been ignored, the delay in diagnosing endometriosis has been extended even further.
On and on it goes.
By the time I see my patients, they are often already receiving Endone (a narcotic) for a condition that has not even been diagnosed. Similarly, Panadeine (a mixture of codeine and Panadol), and Panadeine Forte are a prescription only medication in Australia are the only form of relief she gets and in limited quantity (perhaps rightly so).
Freaked out by the possibility of their patients getting addicted to codeine through the use of Panadeine, general practitioners simply won’t prescribe it. Sometimes the patient is sent away with very little analgesia at all.
But the patient, your loved one, is still in pain, still misses school or work, and still does not have a diagnosis. “Let’s try Ponstan next,” says the next general practitioner. Not a bad idea, but the general practitioner does not really take the time to explain that Ponstan should be taken before a period starts. Why? Period pains are, in part, caused by the release of prostaglandin (the same hormone that nature uses to initiate labour and is also used in a gel form to induce labour). If you have Ponstan at the correct dose before the period starts, then cramps, bleeding, and pain are decreased. So, make sure she is taking the prostaglandin correctly! At least she will get some benefit.
But that’s not the whole story. I am assuming here that your loved one still does not even have a provisional diagnosis and still has not had a laparoscopy. Don’t forget, at the beginning of this book I told you that the average delay in diagnosis for endometriosis worldwide is between nine and ten years. This is beyond belief, and it still astounds me that a patient can see so many general practitioners and still not hear the word endometriosis. By the way, I repeat that this situation does not just happen in Australia, the United States, or Europe—it’s worldwide. Worldwide there is a nine- to ten-year delay!
Pretty scary stuff, especially when the patient is already relying on some seriously hard-core drugs for pain relief. Some of these drugs are addictive, and people do die from their side effects. One state in the USA is currently suing a large company for misleading advertising about codeine. It will be interesting to see the outcome.
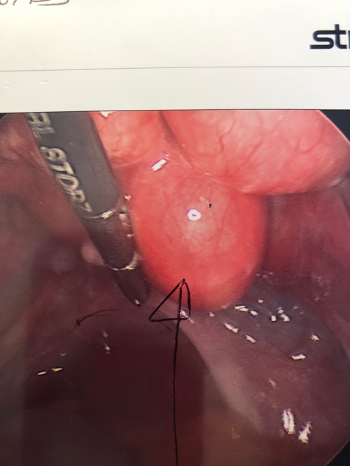
So, I say again, a laparoscopy by an experienced endometriosis surgeon, capable of excisional surgery who will also have an eye out for adenomyosis, is a must.
Cutting out endometriosis or “excisional surgery”, as it is called, not only makes the diagnosis of the disease, but goes a long way towards decreasing the need for narcotic painkillers postoperatively. One of my younger patients recently told me the pain she experienced from surgery was far less than her endometriosis pain.
I try to use the postoperative visit at five days to reassess which painkillers are really needed. I try to avoid more narcotics and codeine. This can be difficult, but we have to make a start. My choice, as outlined previously, is Naprosyn (slow release) 1000 mg, once a day for a maximum of ten days to avoid stomach ulcers. Take it with regular paracetamol, two tablets every three to four hours while awake. In this dosage, paracetamol is very safe, and the combination of an anti-inflammatory and paracetamol makes each pain reliever work better than if just given alone.
Then, at the six-week postoperative visit, I go over it all again, trying to wean her off the anti-inflammatory drug completely. Or, if this is still needed, I try to use it in less frequent and shorter bursts. I add in Nexium 40 mg once a day to prevent the risk of gastrointestinal bleeds if she feels she may need it for a longer duration. Gastrointestinal bleeds are a potentially serious problem with prolonged use of anti-inflammatory drugs.
Tramadol (Utram, Conzip, Rybic ODT, Utram ER)
Tramadol is a restricted opioid-class drug and can also cause addiction.
Tramadol sits somewhere between Panadeine and Endone. Provided your spouse or loved one is not on an antidepressant, it can be used safely. However, if used with antidepressants, it can elicit a rare but serious side effect called the Serotonin Syndrome. Symptoms include high temperature, agitation, tremors, sweating, dilated pupils, diarrhoea, and increased reflexes.
The dose of Tramadol is 50 mg, one to two tablets every six hours. Although it sounds like Panadol, it isn’t. Panadol (paracetamol or Tylenol) can be used in conjunction with Tramadol and in conjunction with an anti-inflammatory.
Sadly, in the immediate postoperative period, and sometimes up until the Mirena(s) has settled in, your partner will need something fairly regularly. Try to drop the Tramadol or any other opioid as soon as possible. Some of these opioids should not be used for more than a few days. If she needs more pain relief than that, it may be an indication that something is wrong.
But hear this—it’s not all bad. In the past year, I have operated on some elite sportswomen: an Olympic swimmer, an Australian team member for international trampolining, and a Paralympian. All had both endometriosis and adenomyosis, and all three remain highly competitive with two Mirenas inserted. Similarly, I have also operated on a highly functioning radio show host. Usually, every patient can get back to their activities, if managed early and correctly, by a group of experts.
All of the women I mentioned above have suffered various similar symptoms to the rest of my patients, but with proper treatment and a concerned ear (mine or yours), we can and do beat this beast that is endometriosis!
Lyrica (Pregabalin)
Lyrica is a drug used to treat neuropathic pain, fibromyalgia, restless legs, generalised anxiety disorder, and epilepsy. Lyrica may take up to a week to be effective.
Lyrica is useful for pain relief on occasions where the patient has had repeated gynaecological insults on their peritoneum (laparoscopies). These repeated insults can damage the nerves on the inside pelvic skin, and patients often report an intense burning pain in their pelvis that may radiate down the legs. Personally, I never start patients on Lyrica myself, but use the service of the pain clinic to decide if it is necessary.
Lyrica can, however, be used prior to surgery in some patients.
What About Sleep Medications?
We all know that if we sleep poorly, for any reason, the following day will be more difficult. Trust me; I’ve been there many times after an interrupted night’s sleep (you just do not function well at all after delivering one or two babies a night). Mothers will tell you the same thing.
So, what to do? One of the first things I ask my patients with chronic pain is, “Do you go off to sleep checking Facebook, Instagram, YouTube, or other social platforms? Do they have a TV in the bedroom?”
If the answer is yes, they probably also have a borderline screen addiction, at the very least. In his 2016 book Glow Kids, psychologist Nicholas Kardaras referenced studies where MRI scans performed on kids watching their mobile phones showed that their brains light up in ways similar to highly rewarding situations such as cocaine use or orgasm during sexual intercourse.
The use of screens up to an hour before bed is not good for anyone’s sleep, but especially someone suffering chronic pain. A blue screen can release the same quantity of dopamine from the brain as with these “pleasurable” stimuli, be they illegal or natural. Dopamine, an excitative hormone, will, if released in increased quantities, slow the release of melatonin, our sleep hormone.
Did you know that Sydney Grammar School in Australia, one of Australia’s premier private schools, has[SBP1] banned laptop computers from school until the last two years of senior school?
Mobile phones, computers, and televisions emit a blue light, and they are addictive and damaging to our sleep. Put them to one side, out of reach, and on silent well before bed and you will sleep better. I suggest putting all devices out of reach.
So, I repeat, I tell my teenage patients to put their mobile phones on silent in another room if possible (no, they won’t die without it), until morning and instead just read ten to twenty pages of a real book, made of real paper. It will help them sleep better, I tell them. Try it yourself.
Getting a better night’s sleep will help patients with chronic pain cope with their pain better the following day and will actually decrease the need for pain relief.
Drugs to Induce a Better Night’s Sleep
Valerian
When I have finished a tough week, need some sleep, and am not on call, I use Valerian Forte. Valerian is a plant and the formula often has other ingredients mixed with it, like vitamin B6 and/or magnesium. Take it about an hour before you want to actually sleep and read twenty or thirty pages of a novel while it is working.
Melatonin
I first discovered Melatonin (5 mg) mixed with vitamin B6 whilst holidaying in Colorado in the 1990s. You could buy it at pharmacies there without a prescription. You can certainly buy it over the counter in airports such as Changi International Airport in Singapore. Melatonin is the hormone secreted by the pineal gland in your brain; it helps regulate your light/dark sleep rhythm.
In Australia, you need a prescription for Melatonin, and a compounding pharmacist will make it up for you. (A compounding pharmacist actually grinds up the ingredients by hand and puts them into a pill press or capsule press.) Plenty of compounding pharmacists are about, or you can order online if you live in a remote area.
Coincidently, I use Melatonin as part of the mix during my IVF cycles for patients. Melatonin acts on the developing egg follicle to help increase the egg’s quality. I prescribe it for days two to twelve of the cycle only. (In effect, when the patient is receiving her FSH[2] injections.) Melatonin, like co-enzyme Q10, is an antioxidant.
Amitriptyline
Amitriptyline is not a hormone, so it does not actually suppress endometriosis (or adenomyosis). However, I find it useful in some patients. Like Lyrica, it is useful for nerve pain when endometriosis itself, surgery, or both have affected the pelvic nerve(s). It also can help women who sleep poorly. I do suggest patients try this medication for the first time on a Friday or Saturday night, provided they are not driving, going out socially, or working, because some women may wake up with a hangover or feeling groggy. The dosage for endometriosis use is much lower than the dosages used years ago to treat major depression. That’s not what we are using it for here.
Amitriptyline can also help settle down an irritable bladder, often seen in cases with endometriosis. It is important, however, that the endometriosis has been surgically removed from the bladder skin before using Amitriptyline for this reason; otherwise, it is just another bandage treatment.
It has been suggested that Amitriptyline may also be of use in women who get cyclic migraine headaches, often starting in the premenstrual phase.
Amitriptyline’s side effects include possible constipation, which can exacerbate the sluggish bowel associated with use of high dose progesterone and other painkillers as outlined above. Always bear this in mind if you know your relative or friend is on both. Movical three sachets [SBP2] at night, works well (as previously described).
The initial starting dose for Amitriptyline is 5 mg. Your partner should not increase the dose if she feels drowsy. However, if she does not have this side effect, the dose can be increased to 10 mg at night. Only increase further after she discusses it with her endometriosis specialist, pain clinic doctor, or general practitioner.
Just so you know, Amitriptyline (an old tricyclic antidepressant), in much higher doses, was used to treat severe depression. But the doses used were around 150 mg a day, not the 5-10 mg we are talking about here. Sometimes the dose is even higher than 150 mg for severe depression. We are talking 5-10 mg only for endometriosis. So, do not let the word “antidepressant” on the drug leaflet put you or her off.
A whole swag of much better drugs than Amitriptyline have been used to treat major depression. So, if yourpartner/significant other is depressed, a newer antidepressant may be necessary, perhaps only for a short time, just like when a Mirena is settling in or to counteract the mood changes that Zoladex or Synarel (mentioned elsewhere) can cause.
Gabapentin (Neurontin) and Its “Mate” Pregabalin (Lyrica)
Both of the above drugs were actually developed to treat epilepsy, but they have the added benefit of interrupting pain signals sent by nerves in the pelvis and elsewhere to the brain.
If your partner or relative has pain she describes as sharp, stabbing, or burning, Gabapentin may help. I personally prefer that a pain specialist (clinic) initiate the use of these drugs, but provided they have a formula to start with, I am very happy to supervise their ongoing use.
Because both drugs can cause sleepiness, drowsiness, and minor weight gain, the pain clinic specialist will usually start with a small dose and work upwards from there as necessary. Gabapentin dosage normally starts at 300 mg a night, but this dose may be doubled under supervision, if needed.
The Pregabalin (Lyrica) starting dose is 75 mg at night, or half that if low BMI and the patient is of slight build. One suggestion I have heard for slight women is to open up the capsule, pour the contents of the capsule into a full glass of water, and drink it. If your significant other starts at this lower dose, just remember it may take her slightly longer to get relief. Again, ask your doctor if this is okay and always start these medications on a weekend (Friday or Saturday night) where she will not be going out, to ensure the dose she takes on Sunday night does not make her groggy on Monday morning, when she may have to drive or operate machinery.
Implantable Nerve Stimulators
Implantable nerve stimulators are truly the realm of the specialist pain physician. The Saint Jude and other brands of implantable pain-reducing devices may be needed in severe cases. These devices are limited to patients with severe pain not relieved by conventional drugs.
I mention these devices for completeness only, because, hopefully, you get your loved one other treatment well before this one is needed.
Before the device is implanted, a test will be performed by a pain specialist to make sure the device will work and it and its electrodes are acceptable to the patient.
Once the pain specialist is happy that your loved one will, in fact, gain pain relief, the device is implanted under the skin and can be switched on and off as necessary. Devices usually last a few years before they need to be replaced.
In real life, as stated above, not many patients with endometriosis and/or adenomyosis will actually need the implant or device, although I do have several such patients in my own practice.
Contraception
Permanent Birth Control
Laparoscopic Tubal Occlusion
Vasectomy
Hysterectomy (only if associated heavy bleeding)