Uterine Fibroid Embolization (for Fibroids)
/Transcatheter uterine artery embolization was first reported in 1979 as a successful treatment for heavy bleeding associated with childbirth. There is a long and successful history of using trans-catheter arterial embolization for the treatment of heavy bleeding in obstetric and gynaecological emergencies. More than 28 years ago in Paris, Dr Rivena and his colleagues noticed that fibroids shrank following emergency embolization for acute bleeding. They then started their programme of UTERINE ARTERY EMBOLIZATION for the treatment of uterine fibroids.
Several years later, the UCLA group (University of California, Los Angeles) started a similar programme. Other centres in the United States followed suit and now the technique is much more accepted and widely used, including at the Wesley Hospital in Brisbane Hospital.
Clinical success (defined as improvement in symptoms of bleeding and pressure caused by a mass), such that the patient does not require further operative therapy has been reported at 85% of costs worldwide. Complications have included infection, pelvic pain, the requirement for antibiotics and occasionally that of a hysterectomy.
Return to work is usually possible within a week or less, with the longest post treatment pain being 2 weeks. The larger the fibroid, the more the post embolization pain. All of my patients have been sent home with adequate pain relieving tablets or suppositories. One third of patients develop symptomatic fever, associated with malaise, anorexia, nausea and vomiting. Approximately 15% of patients may require readmission for these symptoms, but that is actually becoming less common as interventional radiologists become more experienced. Of those patients I have readmitted, the white cell counts were high – 18 000 to 32 000. This is because the fibroid itself dies and this is the body’s reaction to this. If antibiotics are needed for these patients, a broad spectrum or oral antibiotic, combination of Cephalosporin and Flagyl is used.
Pre Procedure Evaluation
It is paramount that every patient be seen by a gynaecologist before uterine artery embolization is undertaken. Patients who have cancer or have a high degree of suspicion of cancer are NOT candidates for embolization therapy.
It is strongly advisable that patients have a laparoscopy and hysteroscopy with biopsy (sampling of the endometrium) to exclude cancer, both of the uterus and of the ovaries. It is most likely however that these biopsies will indeed by negative.
Similarly, if the patient has endometriosis that is not diagnosed, and the patient is embolized principally for pelvic pain, the procedure may be a “clinical failure” – the pain from the endometriosis will continue, even though the fibroid has been shrunk. It would have been easier to diagnose and treat the endometriosis first.
All patients should be counselled extensively regarding the risks, benefits, alternatives and fertility issues regarding Uterine Artery Embolization. This should be done twice – once by the Radiologist and once by the Gynaecologist. In Australia it is a Medicare requirement that the patient has been assessed as suitable for uterine fibroid embolization by a gynaecologist, before the treatment is undertaken.
The alternatives, including no treatment at all, hormonal treatment, myomectomy and hysterectomy, along with transcervical endometrial resection, should be fully discussed, where appropriate.
Thus far, the French and American experience has not reported any cases where fertile women became infertile from embolization. I do suggest all patients, who have had uterine fibroid embolization, and wish to become pregnant have an elective caesarean section at 36 weeks, because of the small, but definite risk of uterine rupture.
Therefore, the standard of care for women with fibroids requiring treatment, remembering many fibroids do not require treatment, should be probably still be a myomectomy rather that UFE. Of course, this could be argued either way.
Technical Details of Embolization Procedure
Uterine artery embolization for fibroids is not a painful procedure – it is about an uncomfortable as having a blood test. Intravenous sedative medicine is usually used during the procedure. Pain killing tablets, suppositories, or injections (if required) are used to control pain after the procedure.
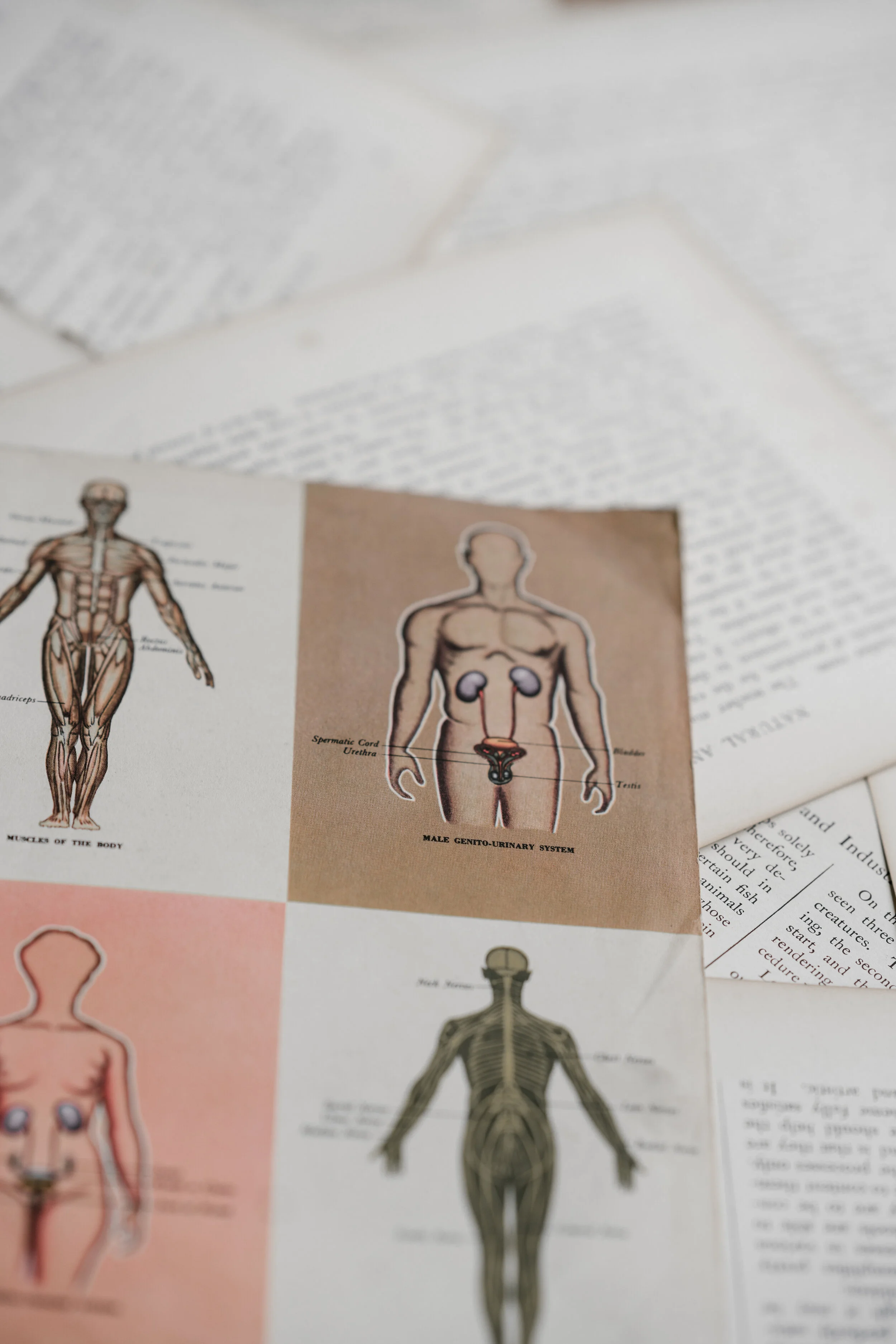
The fine plastic tube (catheter) is placed into an artery in the groin region, after an injection of local anaesthetic, which numbs the area. The artery is entered with a small needle through the numb area, then this is exchanged for the small catheter or pipe. The catheter is guided using an X-ray camera outside the body, which allows visualisation of the catheter and arteries called an image intensifier. X-ray pictures of the feeder arteries (angiograms) are taken to allow accurate assessment, prior to blocking (embolizing) the arteries.
Once the uterine arteries are entered (first one side, then later the other), the blood supply to the fibroids is blocked by injecting lots of tiny particles which lodge within the smallest arteries that supply the fibroid. This is continued until all blood supply to the uterine fibroid is extinguished. PVA is the inert substance which is used extensively around the world for embolization in all parts of the body, eg. brain, lungs, kidneys and fibroids.
Where are the risks? Uterine artery embolization is now very safe and complications are rare. However, the procedure involves blocking the arteries so that there are theoretical risks. Infection and tissue necrosis (dead tissue) have already been mentioned. Unintentional blocking of non-uterine arteries is possible, but rare. Theoretical risks would therefore be damage to other pelvic organs, nerves or the leg arteries. Other risks include allergic reaction to the X-ray dye, or vessel damage where the catheter enters the arteries. All these are now rare in experienced hands.
Post operatively, the aim is to get patients on oral medication for pain relief as quickly as possible before discharge. Patients should have a clinical follow up visit with the gynaecologist in the week following the procedure and an ultrasound scan at 6 weeks and then 6 months, together with a detailed clinical follow up at 6 months. The ultrasound can be done by either radiologist, or an experienced gynaecologist.
At the Wesley Hospital, Dr Graham Tronc (myself) and Dr John Clouston, an interventional radiologist work to help prove that this technique of uterine fibroid embolization was at least as safe as hysterectomies. Dr Clouston has since moved on to run the X-Ray Department of the Royal Brisbane Women’s Hospital. However, a team of other interventional radiologists now work at the Wesley in his place.
Worldwide many thousands of cases of uterine fibroid embolization have been done this way and certainly in Australia we have not lagged behind other countries in this technique. Initial reports from patients suggest that the treatment does offer alternative to the conventional methods of major surgery. Time will tell, but I still continue to recommend this form of treatment to my patients.
Other Gynaecologic Uses for Embolization
Ovarian vein embolization for the treatment of pelvic congestion syndrome.
Pelvic congestion syndrome is characterised by pelvic pain, which has variable intensity and duration. It is usually described as pelvic fullness or heaviness, which is often worse premenstrually. The pain is typically exacerbated by an upright position, pregnancy and fatigue. It is sometimes associated with urinary urgency and constipation. Pain with intercourse and painful periods may also occur.
The syndrome is thought to occur secondary to retrograde flow in ovarian veins which have incompetent “valves”. Women who have had more than one child are particularly at high risk.
Pelvic variscosities (pelvic varicose veins) can commonly be seen on ultrasound. CT scan, trans-uterine venography and ovarian venography are also used to diagnose pelvic variscosities. Of course, they are also seen at laparoscopy. In 1993, Edwards reported the first successful case of embolization procedure for pelvic congestion syndrome. From 1994 to 1997, at least another 23 patients were successfully embolized and since then many more have indeed been embolized. Therefore, based on limited experience so far in the literature, it appears that embolization of the ovarian veins for pelvic congestion syndrome is a safe therapeutic options with few or no reported significant complications. In addition, a good clinical outcome can probably be expected in at least 75% of patients.